Love ‘em or hate ‘em, managed care contracts aren’t going anywhere anytime soon.
They’re the glue that holds the healthcare ecosystem together, but dealing with them can feel a little like removing an appendix.
They’re time-consuming, packed with jargon, and can be a legal minefield if you don’t know what you’re doing.
As a provider, how you navigate these complicated healthcare contracts can make or break your business. But fear not, we’re here to help.
We’ve put together a managed care contract guide written with healthcare pros in mind. So let’s cut through the legal mumbo jumbo and get down to what matters most: making it easy to track and follow through on managed care contracts.
TL;DR
- Managed care contracts are a key component in the healthcare ecosystem, and providers need to be equipped to handle them effectively.
- Contract management software can help providers navigate complicated managed care contracts to ensure their best interests are protected.
What is a Managed Care Contract?
A managed care contract is a legally binding agreement between a healthcare payer and a provider that outlines clear parameters for two essential elements: the compensation the provider will receive for their services and the standards of care they are expected to deliver.
Here is a list of terms often included in managed care contracts:
- Services covered
- Providers who will deliver services
- Timeframe a provider has to submit a claim
- Timeframe a payer has to reimburse providers
- Notice period for terminations or negotiations.
The purpose of managed care contracts is to control healthcare costs while ensuring quality healthcare delivery to patients.

Who Uses Managed Care Contracts?
Managed care contracts are integral in the healthcare system, but navigating them is no easy feat.
Let's take a closer look at who uses these contracts and how they benefit:
- Insurance companies use managed care contracts to create defined networks of providers that offer services at negotiated rates.
- Employers use managed care contracts with health insurance providers to cover the costs of their employee's health care needs.
- Providers, such as physicians and hospitals, benefit from managed care contracts as they provide stability in reimbursement rates and payment models, reducing some of the risks associated with running a practice or hospital.
- Vendors like pharmacies, medical supply stores, and laboratories may also be included in managed care contracts.
- Patients can also benefit from managed care contracts as they help ensure access to quality health care while controlling costs.
Managed care contracts can help you navigate the complexities of healthcare administration.

Types of Managed Care Plans
As a healthcare provider, understanding the types of managed care plans available is essential to ensure you are meeting the needs of your patients and your practice.
Here's a brief look at how these managed care plans impact healthcare providers:
| Plan Type | Description |
| Health Maintenance Organization (HMO) | Think of HMO plans like an "all-you-can-treat" buffet with a catch. You get a fixed payment per enrolled member, but you've got to stick within strict referral and service use boundaries. Efficiency is the name of the game here. |
| Preferred Provider Organization (PPO) | PPOs are a bit like an exclusive club. They contract with providers like you to create a network. The bonus for patients is flexibility - they can see providers outside of the network but at a higher cost. You get a larger patient base, but sometimes at a cut rate. |
| Point of Service (POS) | POS plans combine features from both HMO and PPO plans. Patients can decide to stick within a preferred network (like in a HMO), or seek services outside of it (akin to a PPO). As a provider, it means you get the potential for more patient traffic but will need to navigate the varying reimbursement rates depending on whether services are in-network or out-of-network. |
| Exclusive Provider Organization (EPO) | EPO plans keep it simple for members, they can only see network providers unless it's an emergency. For you, that means offering competitive rates and gearing up for higher patient volumes due to the limited network. |
| Consumer-Directed Health Plans (CDHPs) | CDHPs are the frugal cousin in the family, pairing high-deductible insurance with a health savings account. You need to be ready to tackle patient concerns about costs and be mindful of potential care delays or avoidance due to high out-of-pocket expenses. |
| Medicare Advantage Plans | Operating under these plans feels like balancing on a tightrope. Yes, they're provided by private companies but you've got to stick to Medicare's quality and reporting standards. Plus, each plan carries its own specific rules for costs, referrals, and authorizations. It might seem like a complex dance, but for your patients, it could mean more coverage and added benefits compared to traditional Medicare. |
Understanding managed care plans can help providers make informed decisions about which plans to participate in and how to provide quality care to their patients while also managing costs.
Components of a Managed Care Contract
Entering into a managed care contract is important to ensure you can offer quality care to your patients.
These contracts include several key components that outline the terms and conditions of the healthcare services you will provide:
| Covered Services | List of medical services that get included in the contract and covered by the healthcare payer |
| Physician or Provider Responsibilities | The obligations and duties that physicians or providers are responsible for under the managed care contract, such as providing timely and appropriate medical care, maintaining accurate records, and complying with regulatory requirements |
| Provider Networks | The other providers within the network who will deliver services and how they were chosen |
| Payment Models | How much the payer will cover, and the reimbursement schedule of how and when it will be distributed to the provider |
| Utilization Management | How the healthcare provider ensures that payers are using medical services efficiently and effectively |
| Grievance and Appeal | The process for resolving disputes between the healthcare payer and provider |
| Termination Provisions | What could cause a contract termination, and what happens if a contract is terminated, including notice requirements and any penalties or fees |
Knowing what these terms and conditions mean — and what they should include — is essential in making good business decisions.
Issues To Look Out For When Entering or Negotiating A Managed Care Contract
Entering or negotiating a managed care contract is a collaborative process between healthcare administrators and insurance providers. Both parties bring valuable input to the table with the common goal of providing efficient and high-quality healthcare.
Understanding and negotiating the contract's terms isn't 'us versus them' but rather about finding a mutually beneficial agreement.
Here are some key aspects to consider when entering or negotiating a managed care contract:
- Unilateral amendments: These allow payers to change contract terms at will within a given notice period. Healthcare providers should review any proposed changes carefully to ensure they are in their best interest.
- Reimbursement policies: Different payers may have different reimbursement policies that can impact the provider's revenue. Providers should carefully review these policies to ensure they understand the payment models and reimbursement rates for each payer.
- Network requirements: Payers may have different network requirements they must meet for their provider to include them in their network. Providers should ensure they are aware of these requirements and have the necessary credentialing criteria to participate in each network.
- Credentialing criteria: Providers should review the requirements for each payer's network and ensure they have the necessary licenses, certifications, and experience to meet these requirements.
- Utilization management: Payers may have utilization management policies to control healthcare costs. Providers should be aware of these policies and work to ensure they are not hindering the quality of care for patients.
- Extended timelines: Managed care contracts sometimes require additional approvals which lead to longer timelines. Start working on managed care contracts early and be aware of any extra stakeholders involved in the process.
Knowing what to look out for can give your organization an edge and help ensure you and your patients are being taken care of.
10 Best Practices for Effective Managed Care Contracting
To ensure successful managed care contracting, healthcare providers should follow these best practices:
- Research the market and understand the current trends, regulations, and reimbursement rates.
- Define your goals for entering a managed care contract, such as increasing patient volume or improving revenue streams.
- Evaluate risks like impact on patient volume or reimbursement rates, increased administrative burdens, or obligations that impact your autonomy.
- Review the terms of the contract, including reimbursement rates, covered services, and utilization management policies, and negotiate any changes as needed.
- Monitor contract performance and track key metrics, such as claims submission and denial rates, to ensure compliance with the terms of the contract.
- Carefully review the contract requirements to ensure they have the necessary resources and capabilities to meet them.
- Establish clear roles and responsibilities for all parties involved in the management of the contracts.
- Involve key stakeholders from different departments, such as finance, operations, and clinical services.
- Ensure compliance with all relevant laws and regulations, such as HIPAA and Stark laws, and seek legal advice as needed.
- Maintain a positive relationship with the payer and work collaboratively to ensure the contract benefits both parties.
Taking these steps can make a world of difference when entering or negotiating a managed care contract.
Contract Management Software For Managed Care Contracts
Healthcare contract management software can be valuable for providers looking to streamline their managed care contract processes and ensure compliance with contract terms.
Here are some ways contract management software can help providers with managed care contracts:
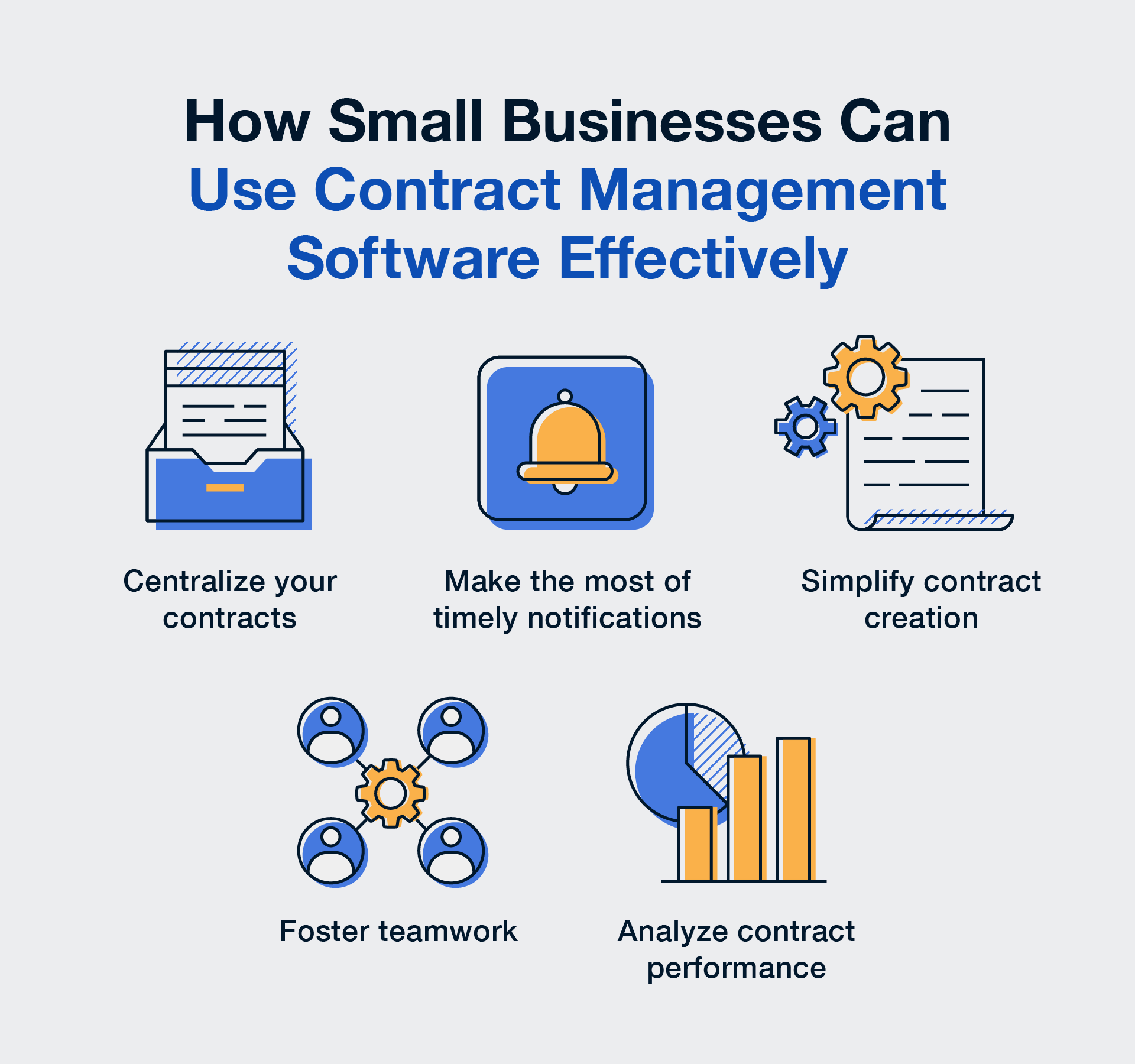
- Improved Organization: Using contract management software, providers can keep all their contracts, schedules, policies, and amendments in one place. This single source of truth makes it easier to find and access the information they need.
- Increased Efficiency: Contract management software can simplify repetitive tasks like manual data entry or sending reminders to stakeholders, freeing up time to focus on more important stuff, like delivering quality patient care.
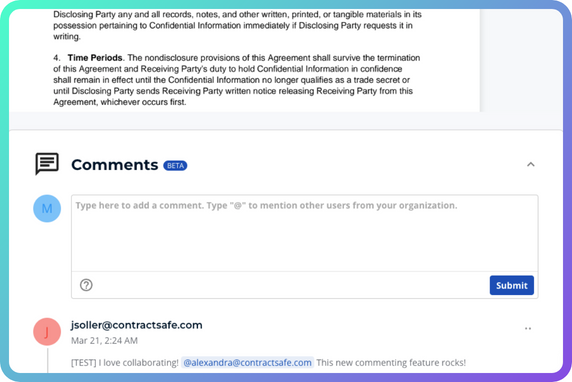
- Better Collaboration: Assigning roles and permissions to different team members and stakeholders can streamline collaboration, ensure everyone can access the right information, prevent unauthorized changes, and ensure patients’ health information (PHI) is protected. It can also easily inform colleagues of new contracts, or changes to existing contracts or policies.
- Enhanced Compliance: Contract management software provides bank-level security, ensuring that sensitive contract information and PHI are protected from unauthorized access or cyber threats.
- Easier Audits: With contract management software, providers can keep a clear record through every stage of the contract management process, including every version of a contract, who was involved in the creation or editing of a contract, and who has accessed the contract.
- Actionable Insights: Detailed reporting on contract activity and performance can provide providers with valuable insights into their operations, helping them identify areas for improvement and optimize their contract management processes for better outcomes.
- Date and obligation management: Managed care contracting may involve tight submission deadlines to submit claims, and missing those dates could lead to claim denials. With contract management software, providers can add payment due dates to keep track of the completion status of payments.

Say Goodbye to Contract Chaos with ContractSafe
Are you tired of struggling to keep track of your managed care contracts? Want to improve the efficiency and accuracy of your contract management process?
Look no further than ContractSafe!
Our contract management software streamlines your work, improves collaboration, enhances compliance, and provides greater visibility into the status of your contracts.
See for yourself how ContractSafe can revolutionize managed care contracting.