HIPAA. Just saying it sends chills down the spines of healthcare legal teams across the United States.
If this is your first run-in with it, HIPAA stands for the Health Insurance Portability and Accountability Act, and it's the law of the land when it comes to protecting medical data. It's one of the most important pieces of legislation ever passed in the healthcare industry. And it can be kind of intimidating.
Protecting patient data is at the core of the regulation, and mistakes can be extremely costly. But don't let all that scare you off — we got your back.
We've put together the most comprehensive HIPAA compliance checklist for 2025, packed with new and pending rule updates, and best practices to keep you and your team safe from the regulatory powers that be.
TL;DR - What You Need to Know About HIPAA in 2025
- HIPAA compliance is mandatory for protecting patient data and avoiding fines
- Noncompliance can carry steep fees (up to $2.1 million per violation) and result in reputational damage.
- 2024 & 2025 proposed updates focus on faster patient data access, expanded privacy protections, and cybersecurity enhancements.
- A strong compliance plan will keep regulators at bay and your business running smoothly.
What Is HIPAA Compliance?
HIPAA compliance means making sure you, your organization and your business associates follow all the rules outlined in HIPAA's Privacy, Security, Breach Notification, and Enforcement Rules.
So who needs to be HIPAA compliant? Short answer: Everyone handling health data.
Longer answer:
Covered entities
- Hospitals
- Healthcare providers such as doctors, dentists, therapists, chiropractors, pharmacists, etc
- Health insurance providers
- Healthcare clearinghouses
Business associates
Business Associates are anyone handling PHI on behalf of a covered entity:
- Data storage firms
- Cloud service providers
- Billing companies
- Attorneys and accountants handling medical records
- Technology vendors whose platforms interact with systems handling electronic PHI
The entire point of HIPAA is to protect patients from unauthorized access or disclosure of their protected health information (PHI) or electronic Protected Health Information (ePHI). So while compliance can be a little bit of a hassle, it's most certainly a good thing.
Now let’s get into the nitty-gritty.
The 5 Core Rules of HIPAA Compliance
- The Privacy Rule
- Patients must have access to and control over their health information
- Organizations must implement policies restricting access and unauthorized sharing
- Healthcare providers must provide a Notice of Privacy Practices (NPP) explaining data usage
- Recent Addition. This new rule requires covered entities to get a signed confirmation (attestation) before sharing any reproductive health information. This ensures that the information is only used for legally permitted purposes.
- The Security Rule
- Covered entities and business associates must implement administrative, physical and technical safeguards to protect ePHI.
- Data must be encrypted both in transit and at rest.
- Access control measures (e.g., role-based permissions, multi-factor authentication) must be implemented.
- Breach Notification Rule
- If there's a data breach, you must notify:
- Affected individuals promptly
- Health and Human Services (HHS) within 60 days
- Media, in cases of large-scale breaches
- If there's a data breach, you must notify:
- The Omnibus Rule
- Extends HIPAA compliance and liability to business associates
- Covered Entities must sign Business Associate Agreements (BAAs) with vendors handling PHI.
- All HIPAA-covered entities must provide a notice of privacy practices to their patients.
- The Enforcement Rule
- Covered entities must have an internal compliance program to investigate and address violations
- Penalties for HIPAA violations where increased in 2024 with a maximum annual penalty of $2.1 million per category.
- Up to 10 years in jail for willful misuse of PHI
To be HIPAA compliant, you’ll need to take appropriate measures to ensure that your organization is meeting these requirements.
Why HIPAA Compliance Is Important
Well, for one, it's the right thing to do. By adhering to the requirements of HIPAA, you're protecting your patients.
If you ask your legal team, though, they might mention that there is another pretty big reason to remain compliant: noncompliance is expensive. Like, really, really expensive.
In fact, the average cost of a data breach in the healthcare industry exceeds $10 million. That includes Department of Health and Human Services fines of up to $2.1 million per violation.
Noncompliance can also damage your organization's public image. After all, patients want to know that their health data is safe and secure.
Accidents happen — and they can be costly. But individuals knowingly violating HIPAA regulations for personal gain could face even steeper penalties. We’re talkin’ up to 10 years in the clinker.
If you don't keep up with HIPAA regulations, you're not only putting your patients at risk, but you’re also risking massive fines and a potential loss of business.
Potential Updates to HIPAA in 2025
With the healthcare industry facing increasing cybersecurity threats and evolving privacy concerns, new HIPAA rules are being proposed to address these challenges. In 2024, 186 million user records were affected by breaches involving PHI, setting a new record in the healthcare sector. The proposed updates to the Security Rule in 2025 include:
- mandatory encryption of ePHI
- requiring multi-factor authentication for accessing systems with ePHI
- annual security audits with vulnerability scans every 6 months.
- expanded obligations for business associates to ensure compliance with updated security measures
The proposed rule is open for public comment until March 7, 2025, with a final rule expected later in the year.
Enforcement actions are also expected to increase in 2025. The Office for Civil Rights (OCR) is introducing HIPAA audits, with a strong emphasis on compliance failures related to patient access requests, risk assessment procedures, and cybersecurity measures. Organizations that delay responding to patient record requests or fail to implement required security protocols could face steeper penalties.
By staying ahead of these updates and ensuring compliance with the latest requirements, healthcare organizations can reduce their risk of financial penalties and protect the integrity of their patient data.
The Ultimate HIPAA Compliance Checklist
Wondering how you can make sure your organization is compliant with HIPAA regulations? Don't worry, we're here to help.
We've put together a handy HIPAA compliance checklist to make sure you cover all the bases:
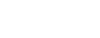
1. Conduct a Risk Assessment
The first step to HIPAA compliance is conducting a comprehensive risk assessment based on the five rules we mentioned above.
This means evaluating the technology and devices you use, assessing your policies and procedures, analyzing the data that flows in and out of your system, and understanding how to secure sensitive patient information.
Remember:
- Patients must have access to their PHI
- PHI must be stored securely
- You must provide a notice of privacy practices to all patients
- You need a process in place to notify patients if their PHI is compromised
- You need a comprehensive procedure in place to investigate complaints of noncompliance
Risk assessments should be repeated on a regular basis so you can make sure you're up to date with the latest regulations and best practices.
Here are a few questions you can ask in your HIPAA risk assessment:
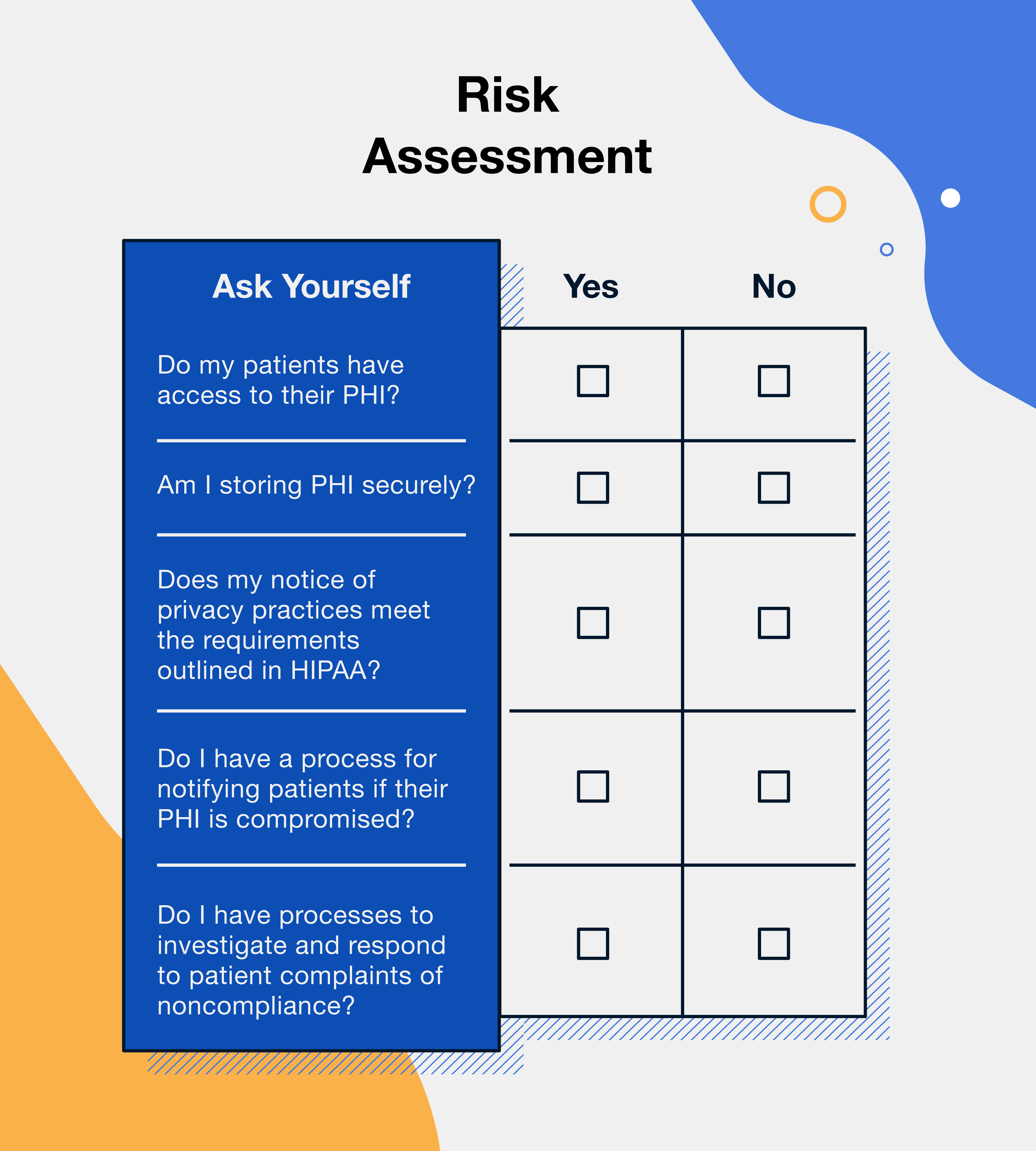
2. Implement Security Safeguards
Once the risks to PHI have been identified, you must develop a comprehensive security plan to address them. This security plan should include physical and digital safeguards designed to protect PHI and ePHI from unauthorized access, use, or disclosure.
- Physical safeguards are things like locked doors and file cabinets, security cameras, and shredders for destroying confidential information.
- Digital safeguards include things like software with bank-level security, contract management solutions that allow you to set permissions and roles, password protection, two-factor authentication, encryption, and firewalls.
You'll also want to perform due diligence on your business associates like cloud storage providers, vendors, or anyone else that may have access to or be in charge of PHI to ensure they're complying with these safeguards. Make sure security provisions are outlined in contracts and review them regularly in case you need to update them.
Here are a few questions you can ask to ensure your HIPAA security safeguards are satisfactory:
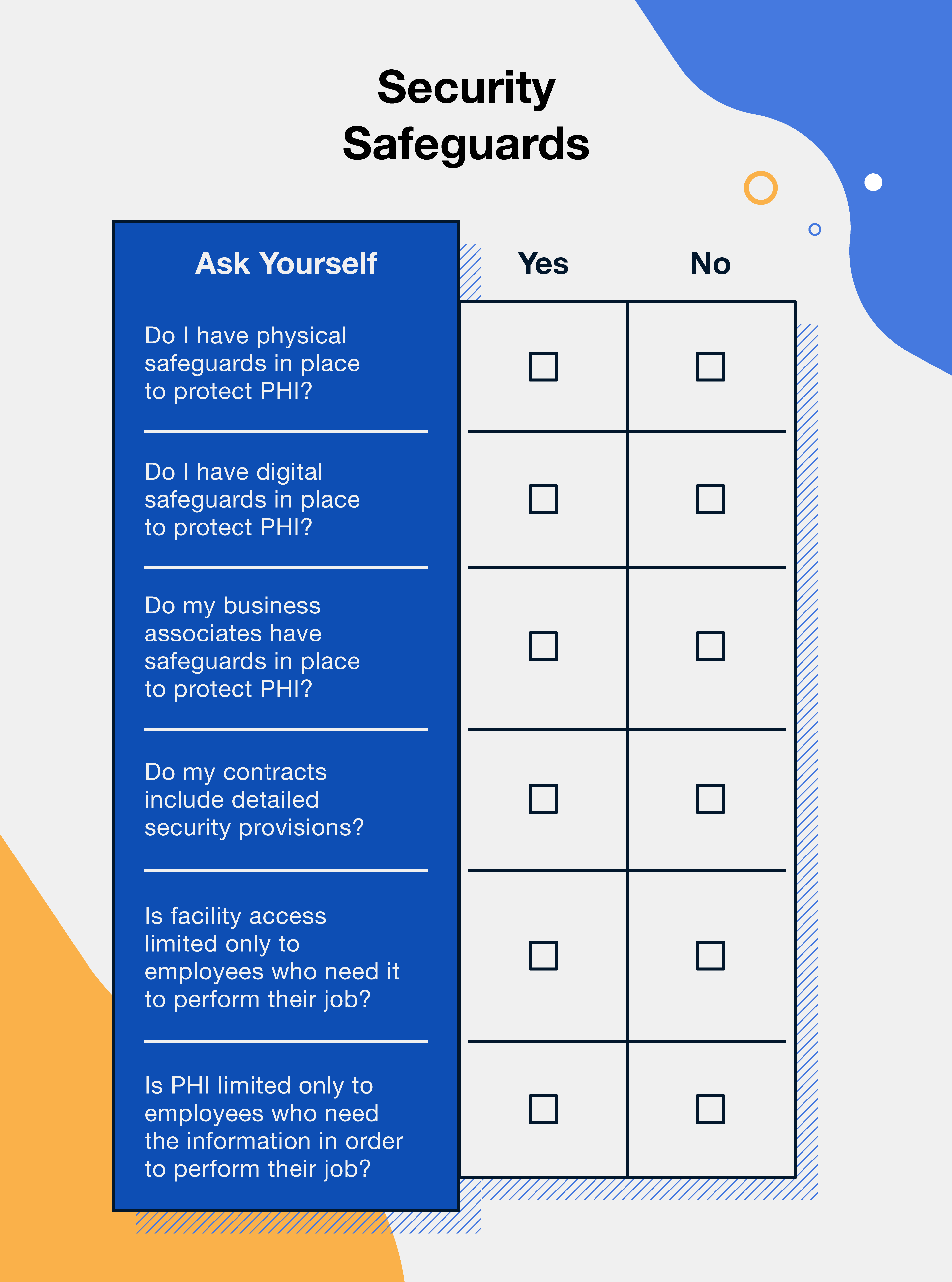
3. Establish Administrative Policies and Procedures
Written policies and procedures are the lifeblood of organizational compliance.
Create a policy for routine system maintenance and monitoring, incident reporting, and how to handle violations.
You'll also want to outline appropriate sanctions for employees who violate HIPAA rules. Make sure everyone in the organization knows who is responsible for ensuring compliance and when any audit reports or assessments must be completed.
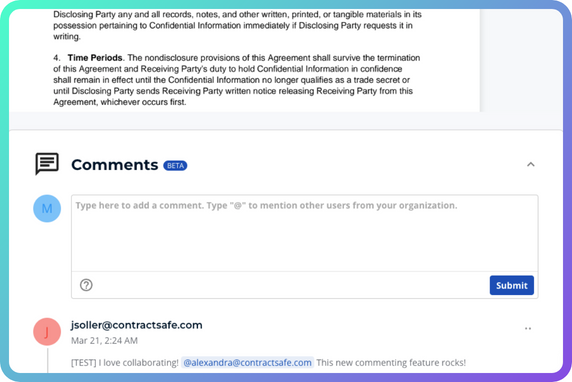
Finally, arm your compliance officers and contract managers with a top-tier contract management solution.
Software with the ability to set permissions and roles for specific documents will ensure that PHI is safe from prying eyes and allow you to terminate access when employees change roles, leave the organization, or move on to another patient.
Here are a few questions you can ask to make sure your policies and procedures are adequate:
4. Create a Contingency Plan
We all know Murphy's Law: Anything that can go wrong will go wrong.
That's why it's important to prepare for anything and everything that could put PHI at risk.
Here are four key goals every HIPAA contingency plan should accomplish:
- Establish clear lines of communication: Define who will be responsible for contacting the proper authorities, communicating with patients and healthcare providers, and notifying employees in the event of a violation.
- Outline appropriate responses: Have a plan for responding to violations, taking corrective action, and responding to media coverage.
- Guarantee quick response times: Set deadlines for responding to violations and resolving issues as quickly as possible. Delaying action runs the risk of further damage and could result in more expensive fines.
- Test your plan regularly: Conduct drills and tabletop exercises with your staff. By testing your plan regularly, you can identify any weaknesses and make necessary adjustments before an actual emergency occurs.
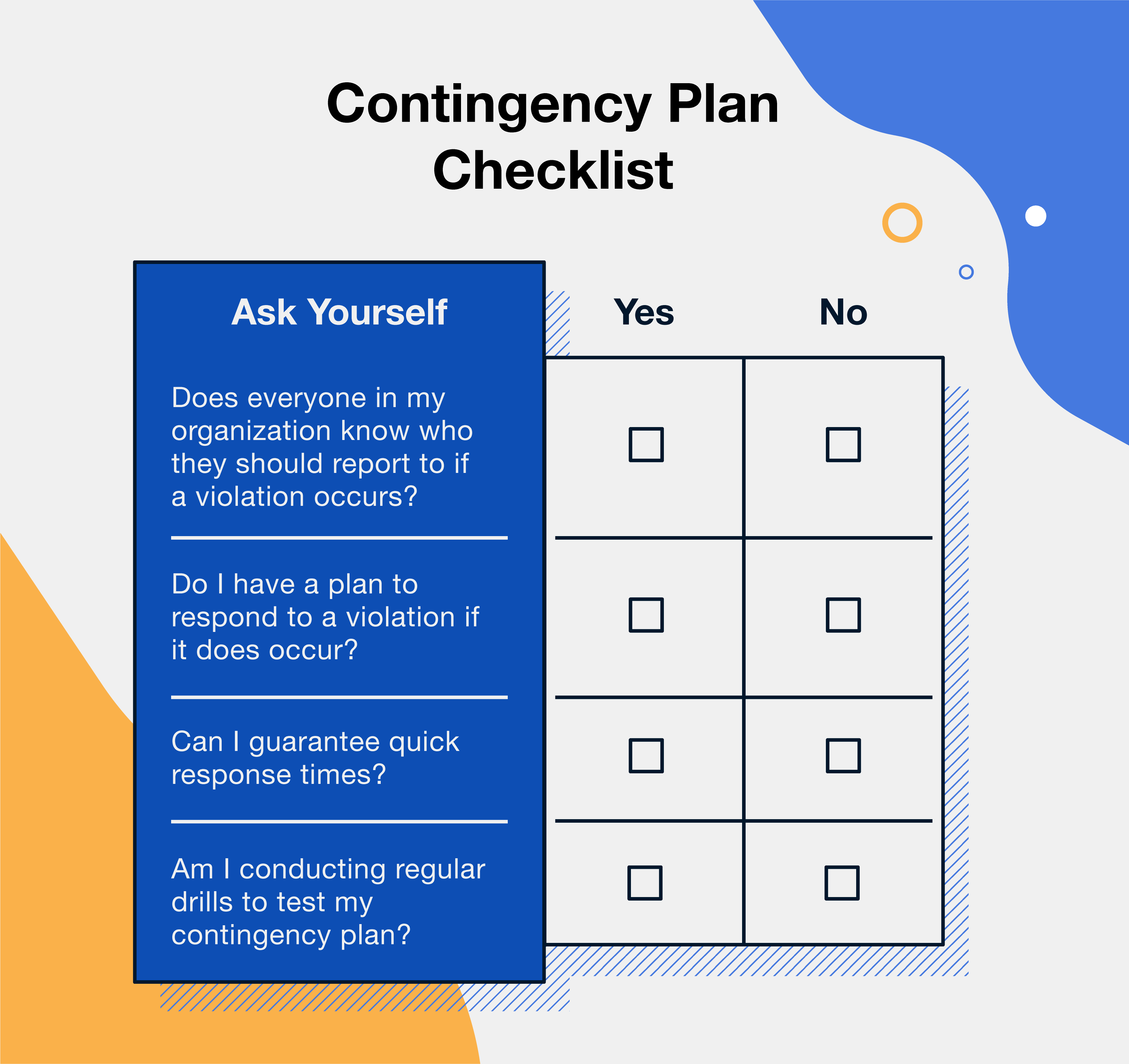
Here are a few questions you can ask to make sure your contingency plan is sufficient:
5. Train Your Employees on HIPAA Compliance
Ever heard this one? “For the best return on your money, pour your purse into your head.”
When Ben Franklin said that, he wasn't talking about HIPAA, though he could have been!
Not only is training required under HIPAA law, but it's also got a great ROI.
Remember, a data breach could result in an eight-figure loss, so training your team on how to prevent a breach, or mitigate the damage if one does occur, could help you save a pretty penny.
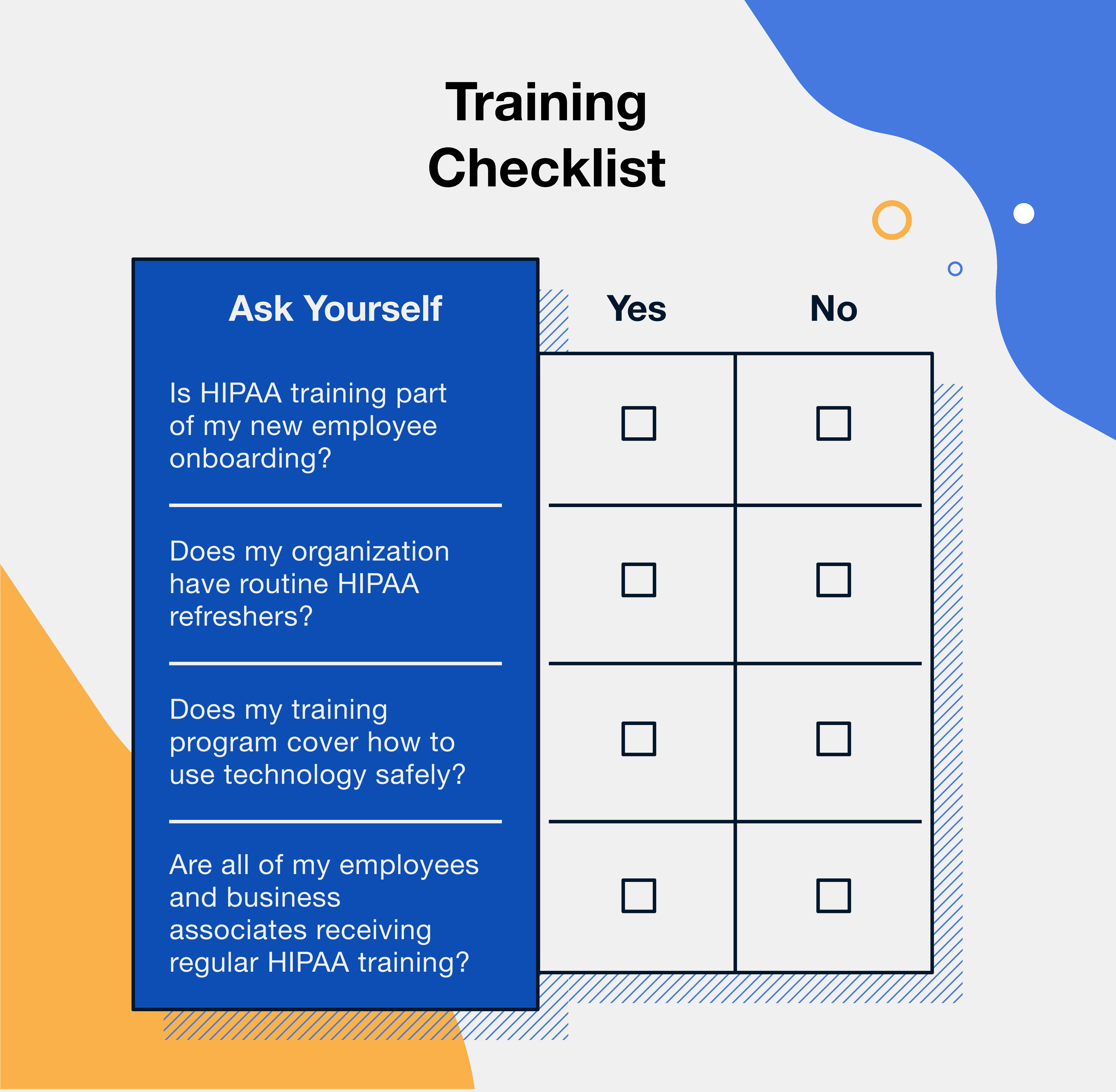
So, who needs training? Everyone! That includes employees and business associates who handle PHI. And it shouldn’t be a one-off onboarding session, either. You’ll need to make sure you have routine refreshers as well. Here's a quick list of topics your training should cover:
- Overview of HIPAA rules
- Guidelines for keeping data secure
- Proper handling of PHI
- Reporting security breaches
- How to use HIPAA-compliant software
- Cybersecurity best practices
- Risk assessment protocols and procedures
6. Document Everything
Hansel and Gretel left breadcrumbs to find their way home. You might consider taking a page from their book!
When it comes to keeping your organization compliant, having a paper trail and a secure, organized repository is everything.
Compliance audits are inevitable, so compiling regular reports showcasing your compliance efforts is a must.
These reports should cover things like:
- All training that has taken place
- Policies and procedures
- Security measures
- Incident reports and complaints
- Any disciplinary actions taken for noncompliance
Hansel and Gretel made it home safely, and if you audit-proof your organization, you will, too!
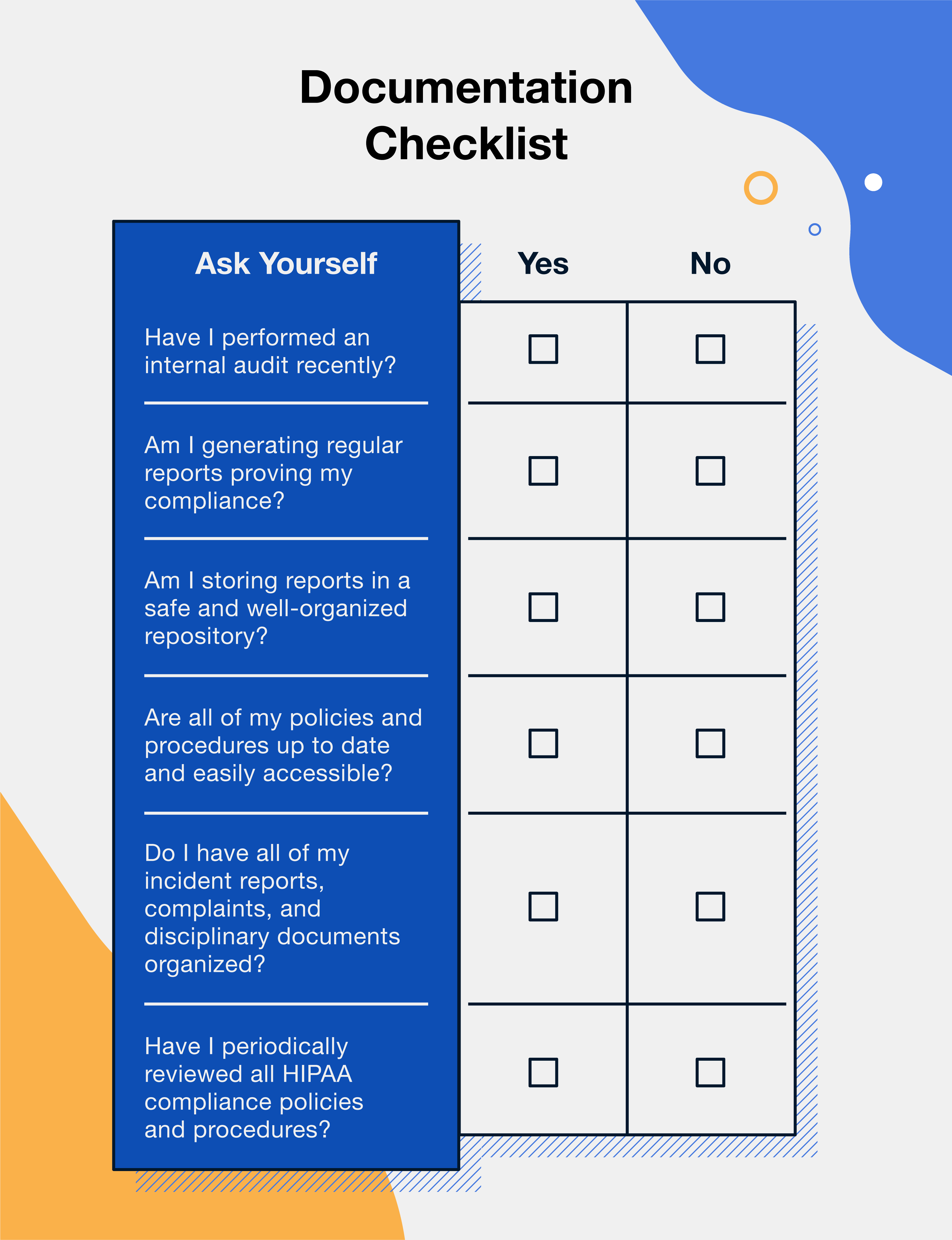
Here is a quick checklist to ensure you’re documenting everything you need to be documenting:
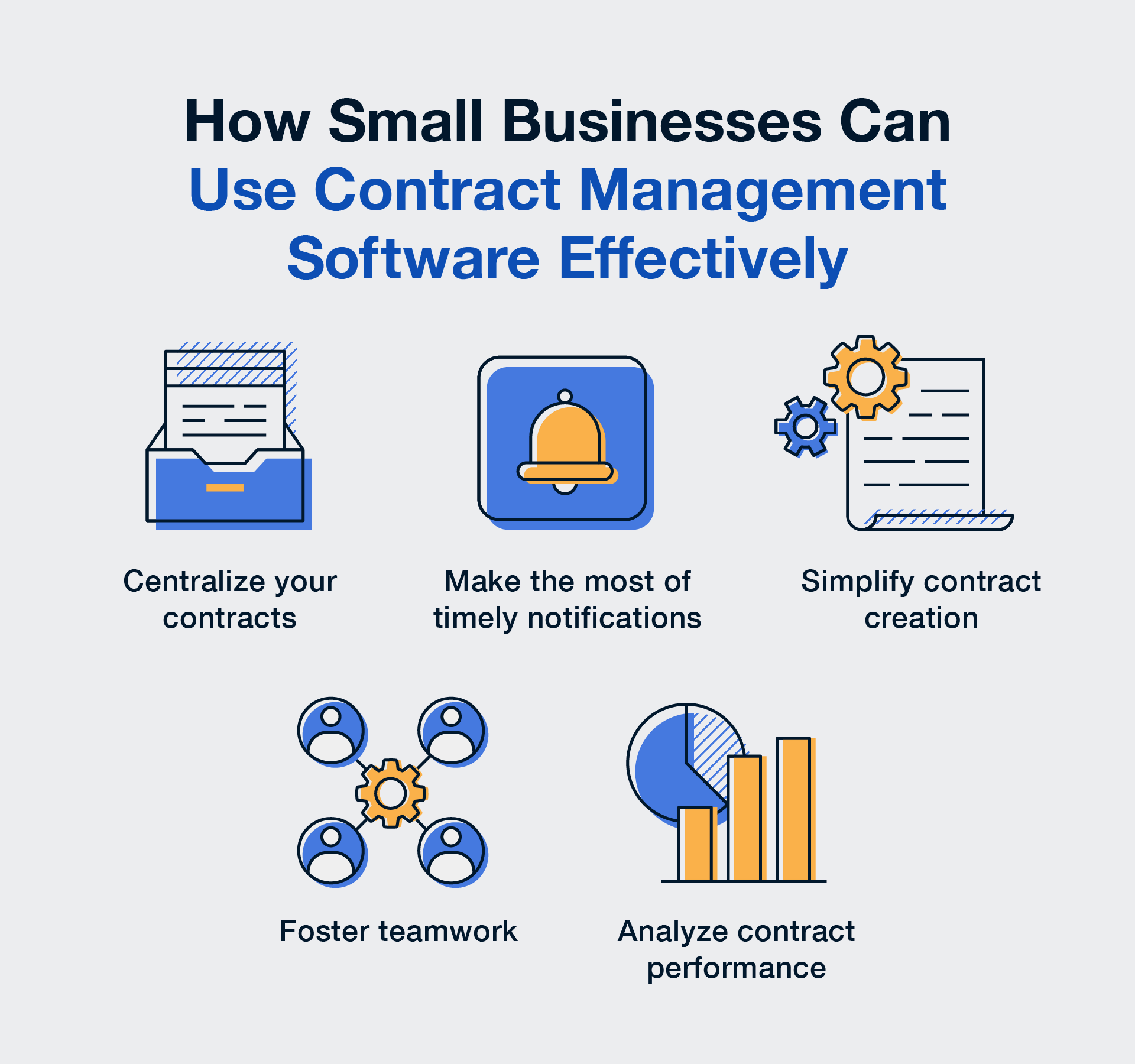
7. Use the Right Software
You know that old saying, “you’re only as good as your tools”? Well, it couldn’t be truer when it comes to HIPAA compliance.
And these days, it's all about software. HIPAA-compliant contract management software.
Whether you're managing contracts or organizing patient files, you need a system that fulfills at least a few basic requirements:
- Secure against unauthorized access
- Able to encrypt or otherwise protect sensitive data
- Accurately track who has accessed the data and when
- Accessible by only authorized personnel
- Ensures the confidentiality and integrity of all PHI
- Backs up all ePHI to ensure it can be accessed by patients in case of emergency
Remember: If you’re using a third party as your technology provider, you will need to do your due diligence to make sure their systems are in tip-top shape and following the best practices outlined by the Department of Health and Human Services.
Here’s a quick checklist to ensure you’re following the best tech practices possible:
HIPAA Compliance Has Never Been Easier
Contract management software makes HIPAA compliance a walk in the park. With automated processes, detailed reports, user permissions and roles, and a secure, centralized digital repository for all your HIPAA documents, you can be sure you’re meeting the standards of compliance.
Want to see how you can beef up your compliance efforts today? Poke around ContractSafe's healthcare-specific contract management features during a free trial!